Abstract

Background. The tendency towards thrombosis in myeloproliferative neoplasms (MPNs) is linked to the JAK2-mutant clone which leads to hypercellularity and functional interplay between abnormal erythrocytes, platelets, leukocytes and dysfunctional endothelium. The resulting cell activation that also involves stromal cells in their microenvironment, has been shown associated with chronic, systemic, subclinical pro-inflammatory state, and has been implicated in the pathogenesis of thrombosis in MPN. Neutrophil to lymphocyte ratio (NLR) is a novel inflammatory marker found to be associated with the severity and prognosis of cardiovascular diseases but there is little evidence for its prognostic significance in MPN. We investigated whether NLR could predict the onset of arterial and venous thrombosis in polycythemia vera (PV).
Methods. Subjects of this study were 1508 patients included in the ECLAP trail with NLR evaluation available. In addition to standard statistical methods, we used proportional hazards additive models (GAM) as they can provide an excellent fit in the presence of nonlinear relationships, for the prediction of total, arterial and venous thrombosis as smooth functions with cubic splines of different blood parameters.
Results. After a median follow-up of 2.76 years, 169 thrombotic events (10.3%) were objectively diagnosed and analyzed: 87 arterial (MI, Stroke, TIA, PAT) and 88 venous thrombosis (DVT±PE, superficial thrombophlebitis).
In univariate analysis, arterial thrombosis was associated with age (p=0.003) and previous thrombosis, especially if arterial (p<0.001), and with the presence of at least one cardiovascular risk factor (p=0.009). No association between baseline platelet and leukocyte counts and NLR with arterial events was found. Conversely, in venous thrombosis, beside age (p=0.039) and history of venous thrombosis (p<0.001), additional risk factors were low hemoglobin (p=0.039) and increasing values of NLR (p=0.002) resulting from a simultaneous increase of neutrophils (p=0.002) and to a decrease of absolute number lymphocytes (p=0.002).
To predict outcomes, we tested total leukocytes, neutrophils, lymphocytes, platelets and NLR by GAM to evaluate their trend in continuous scale of thrombotic risk. A significant association between the risk of venous thrombosis and the progressive lower counts of lymphocytes (p=0.002) emerged, leading to increase the NLR values (p=0.005). However, given the greater precision of the NLR estimates and the markedly wide confidence interval of lymphocyte counts estimates, NLR was used in multivariate model. Conversely, neither absolute values of neutrophils and lymphocytes nor NLR were found associated with arterial events.
In multivariate model, adjusted for age, gender and treatments at baseline, the risk of venous thrombosis was independently associated with previous venous events (HR=5.48, p ≤0.001) and NLR values ≥5 -the best cut-off resulted applying the Liu's method (HR=2.13, p=0.001). NLR effect for total venous thrombosis was not modified by excluding superficial venous thrombosis (HR=2.90, p=0.001) in a sensitivity analysis. Older age (i.e., ≥65 years, HR=1.88, p=0.005) and previous arterial thrombosis (HR=1.92, p=0.003) retained the prognostic statistical significance for arterial thrombosis.
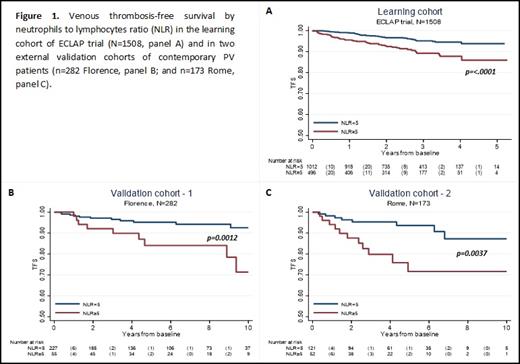
Our learning cohort findings, indicating a correlation between NLR values and venous thrombosis, have been validated in two Italian independent external cohorts (Florence, n=282 and Rome, n=173) of contemporary PV patients (Figure 1).
Conclusions. The NLR is an inexpensive and easily accessible test compared to other inflammatory markers. We found that NLR-alone is an independent predictor of venous thrombosis and could be included in a new scoring system. In addition to guiding the stratification of thrombotic risk, these data confirm that inflammation is a relevant target of antithrombotic therapy in PV.
Vannucchi: Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees; Incyte: Honoraria, Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees. Barbui: AOP Orphan: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal